Pancreatic Islets Management System
Increasing patient access to treatment for diabetes
System Engineering and Design, Sensor Array, Control Software, Risk Management
The global incidence of diabetes mellitus is on the rise.
Since the late 1990s, medical practitioners have been refining a procedure to treat Type 1 diabetes, known as the Edmonton Protocol, during which patients receive a transplant of pancreatic islets – the cells responsible for insulin production.
Following a successful operation, some patients report life-changing results. Their bodies once again produce and regulate their insulin levels and they are no longer dependent on daily injections.
However, the success of the transplant operations and the number conducted are affected by the poor supply of pancreatic islets.
The islets are currently stored, transported and delivered using blood bags and associated infrastructure. This process and the initial harvesting steps can result in cell damage, leading to less than 10 per cent of the cells successfully engrafting in the recipient.
Cambridge Medtech Solutions are working with Loughborough University’s Centre for Biological Engineering and the Institute of Cellular Medicine at Newcastle University – international experts in the field of pancreatic islets transplantation – on the development of a novel technology that will significantly improve the delivery of donated pancreatic islets.
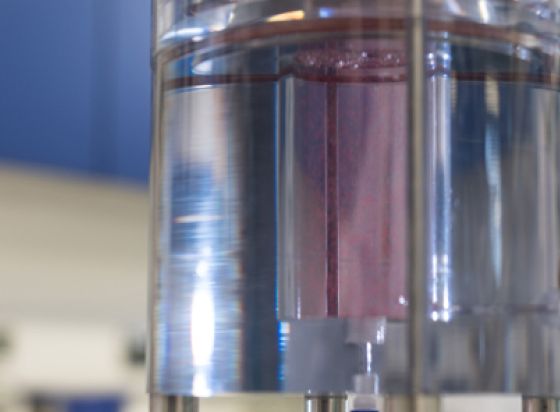
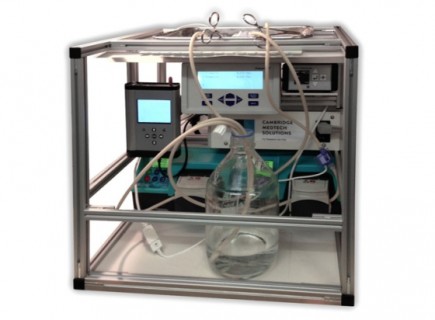
The Pancreatic Islets Management System (PIMS) is intended to provide optimal storage of and transportation conditions for donated cells as well as automated delivery.
Its design ensures constant monitoring and control of the key factors affecting tissue health, including temperature regulation and a steady supply of oxygen and circulating media.
This means that a higher quantity and quality of islets are likely to arrive at theatre and be transplanted.
A platform technology, PIMS has been developed to deliver donor tissue, but is compatible with emerging technologies – including autologous treatments, bio-printed islets and other organoids.
Cambridge Medtech Solutions are responsible for all aspects of medical device engineering and design (including sensor array and control software), risk management, and supporting the on-going laboratory work and regulatory positioning.
Background Info on Hypoglycaemic Type 1 Diabetes
There are currently over 320,000 patients in the UK with type 1 diabetes and this number is predicted to rise in the UK to 652,200 by 2035 (Diabetes UK, 2014).
Worldwide, the total number of patients with diabetes is estimated at ~347 million (WHO, 2014), with ~21 million patients suffering from type 1 diabetes (~6 % of diabetic population).
Type 1 diabetes is normally treated by administration of insulin injections. Approximately 90% of all patients who receive insulin treatment have experienced hypoglycaemic episodes. Ten percent of T1D patients have impaired awareness of hypoglycaemia, and ~ 5% of patients experience more than 7 serious hypoglycaemic events per year (corresponding to ~14,000 patients in the UK). Such episodes often require outside intervention, and can, in severe circumstances, require hospitalisation and may result in loss of consciousness and coma. There is thus a high unmet medical need for improved therapeutic strategies for this patient population.
Transplantation of islets isolated from donor pancreas to patients with type 1 diabetes have demonstrated improved hypoglycaemic awareness.
However, current techniques and technologies expose the cells to a variety of risks – for example, hypoxia / anoxia, flow shear stress, physical shocks and thermal shocks (including freezing and thawing) – which may lead to cell damage, loss of function, or cell death.
Pancreatic islets are organoids found in the pancreas, and they provide patients with glucose control that is both effective and long term.
Insulin-producing beta cells make up around 70% of the content of an islet. The remaining 30% is largely made up of alpha and beta cells, which, respectively, produce the peptide hormones glucagon and somatostatin. Glucagon and somatostatin are both involved in the feedback system that regulates blood sugar levels.