Shisa Kanko could reduce mistakes and save lives
May 10, 2020
Shisa Kanko is a proven method of reducing human error. This valuable tool could be implemented across the NHS and pharmaceutical industry to save time, money and lives during the coronavirus pandemic and in the future.
Why do we need Shisa Kanko?
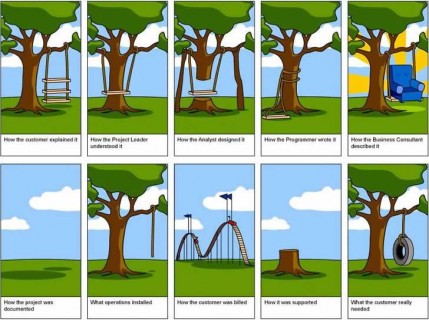
Humans are fallible, we all make misteaks. Like that one, the majority of these mistakes are of little importance, but sometimes the consequences are significant. In industry and healthcare, human error impacts finances, efficiency, deadlines, reputations and lives. We are all equally capable of seeing what we want or expect to see at times, rather than what is actually there. Any method that is proven to minimise the potential for error is worthy of our attention.
Many years ago I lived in Japan and was aware of Shisa Kanko but I hadn’t appreciated its validity at the time. I recently happened across a post written by Malcolm Finlay, a Consultant Cardiologist working with the team building the Nightingale Hospital in London. Unintended human error in this setting could have disastrous consequences. Finlay foresees an increased likelihood of communication errors among tired/stressed individuals communicating through their PPE in a high pressure environment, treating COVID-19 patients. His suggestions to overcome this are three-fold:
- Individuals should introduce themselves at the start of every encounter
- Repeat back all critical data
- Use Shisa Kanko
What is Shisa Kanko and how does it reduce human error?
Shisa Kanko (指差喚呼) is the practice of pointing and calling, and it is used to increase occupational safety. Japan and China’s railway network implemented it to reduce human error, with impressive results. The 1994 Railway Technical Research Institute study revealed an 85% reduction in mistakes when carrying out simple tasks. Consequently, Shisa Kanko was rolled out across industry in Japan.
Shisa Kanko is a behaviour based approach using auditory, kinesthetic and visual stimuli to prevent tasks being carried out with a lack of attention. Instead of functioning on ‘auto-pilot’ to carry out routine tasks, the individual performs a coordinated response requiring him/her to point at the object of the action and call out its status. The process requires focus and attention and reduces the probability of user error.
Scientific research reveals an increase in blood flow to the frontal lobe of the brain when an individual uses Shisa Kanko; the frontal lobe is an area of the brain that controls attention. Shisa Kanko sharpens focus and attention while reinforcing learning and strengthening neural pathways. Incidence of error is drastically reduced, the potential is great.
Potential Applications of Shisa Kanko
Healthcare
The potential for human error across healthcare could be reduced significantly. Examples include: application of PPE, drug dispensing and administration, patient observations, equipment choice and use, selection of syringe/device, area of patient being attended to/operated on, and post surgical removal of swabs and instruments. The list is extensive.
The use of Shisa Kanko could be applied to procedures at every level. Individuals point to the task they are going to complete and say its current status out loud, e.g. (point to figure on screen) “Oxygen sats for patient Mr X, 78%”, (point to chart) “I am recording 78% on the patient’s chart”. Full attention is on the detail of the task.
Nightingale Hospitals
As London’s Nightingale Hospital opens, with others across the country following, systems that prevent error will be vital.
Communication will be restricted by additional PPE, workers will be unfamiliar with each other and the environment, routines will be altered and the situation will be challenging and stressful. Shisa Kanko could improve communication and minimise mistakes.
Never Events
In 2019, NHS England published 435 reported Never events, an increase from 423 the year before. Never events are, ‘serious, largely preventable patient safety incidents that should not occur if healthcare providers have implemented existing national guidance or safety recommendations’.
These events are highlighted and investigated as a learning tool, and their occurrence is indicative of the need for more robust safety measures. Universally practised Shisa Kanko could have a dramatic impact.
Pharmaceutical Industry
Within the pharmaceutical industry, research suggests that as much as 40% of deviations are due to human error, that translates to a lot of time and money wasted. Laboratory techniques can be repetitive and it is too easy to perform repetitive, seemingly mundane tasks without full attention. Unexpected or seemingly accurate data may result from undetected errors earlier in the procedure.
Patient Self-Administration
Non-adherence is a known problem with certain medications, and asthma self-medications are prime candidates, as I have previously discussed. Patients experience symptoms and require medical intervention which could have been avoided through better adherence.
Initial training for patients from healthcare professionals using Shisa Kanko would help patients ‘attend’ to the IFU (information for use) and memorise steps accurately. The result is correct, longer-lasting adherence of the medication and a reduction in symptoms.
The Future
Imagine future training within any industry that includes Shisa Kanko. Not just healthcare but also construction, manufacturing, transport, mining, automotive, energy, and travel. These industries among others could benefit from the application of Shisa Kanko, training individuals to improve attention to the task and reduce human error.
A BIG THANK YOU to the NHS and All Key Workers
Originally published as a LinkedIn Pulse article entitled Shisa Kanko could reduce mistakes and save lives (May 2020)